Where Complex Symptoms Become Clear Strategies.
Clinical Care
Clinical Care
Where Complex Symptoms Become Clear Strategies.
Overview

Overview
Patients presenting with gastrointestinal symptoms often experience concurrent cognitive, neurological, and emotional dysfunction. By collecting real-time, cross-system data, we evaluate how structured interventions perform in real-world care and how they scale beyond it.
Every data point contributes to evidence-driven platforms for trial optimization, drug repurposing, and systems-level care design, turning clinical patterns into scalable solutions.
Irritable Bowel Syndrome: Outcomes Beyond the Bowel
Irritable Bowel Syndrome (IBS) is one of the most frequently encountered GI conditions, but one of the most difficult to treat in isolation. Symptom response often depends on multiple variables: dietary triggers, emotional reactivity, and central processing of discomfort.
Clinical insights include:
- Structured dietary change at Penn Clinical improves both GI symptoms and emotional burden.
- Remote-delivered CBT reduces pain severity and increases functional resilience in outpatient cohorts.
- Symptom-mood clustering predicts optimal pathway for diet vs. CBT selection.
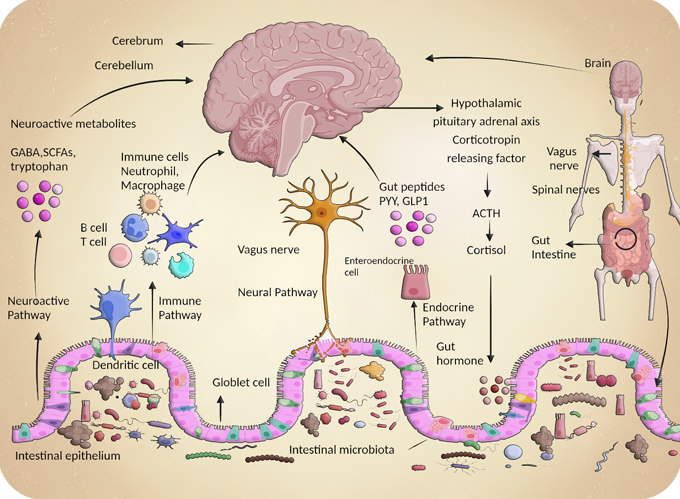
Dysbiosis and Neurodegeneration: New Frontiers
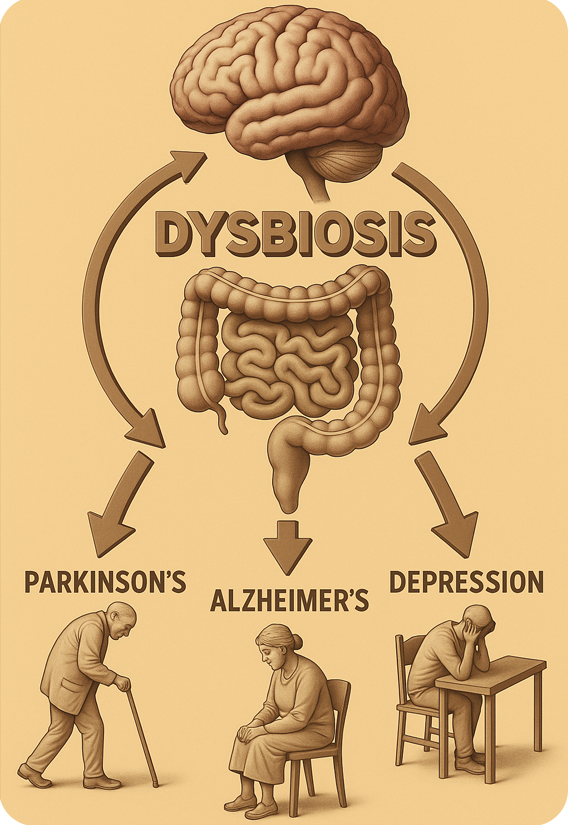
Dysbiosis and Neurodegeneration: New Frontiers
Disruptions in the gut microbiome are increasingly recognized as early signals in neurodegenerative disease and mood disorders. Penn Clinical tracks microbial patterns alongside symptom evolution to better understand these connections.
Observed treatment outcomes show:
- Stool microbiome profiles from Penn Clinical patients reveal dysbiosis patterns preceding cognitive decline.
- GI inflammatory markers correlate with prodromal symptoms in Parkinson’s and Alzheimer’s cohorts.
- Targeted microbiota modulation shows early symptom mitigation in mood-disorder patients with GI overlap.
- New gut-derived inflammatory signatures are emerging as early biomarkers for neurodegenerative risk stratification.
- Microbial composition shifts predict neuromodulator and cognitive therapy response rates in real-world data
Functional Dyspepsia: Not Just the Stomach
Functional Dyspepsia (FD) frequently overlaps with IBS and mood disorders, complicating both diagnosis and management. Fatigue, cognitive strain, and anxiety often shape how patients experience upper GI symptoms.
Functional Dyspepsia: Not Just the Stomach

Functional Dyspepsia (FD) frequently overlaps with IBS and mood disorders, complicating both diagnosis and management. Fatigue, cognitive strain, and anxiety often shape how patients experience upper GI symptoms.
Emerging Findings:
Cognitive load and sleep disruption predict treatment response, based on patient-reported outcomes.
Overlap with IBS necessitates shared diagnostic strategies and modular intervention tools.
Dual-modality care improves both symptom relief and daily functional capacity.
Anxiety and cognitive fatigue scores guide therapy choice in functional GI management.
See how our work drives better patient outcomes.
Emerging Findings:
Stool microbiome profiles from Penn Clinical patients reveal dysbiosis patterns preceding cognitive decline
GI inflammatory markers correlate with prodromal symptoms in Parkinson’s and Alzheimer’s cohorts
Targeted microbiota modulation shows early symptom mitigation in mood-disorder patients with GI overlap
Microbial composition shifts predict neuromodulator and cognitive therapy response rates in real-world data
New gut-derived inflammatory signatures are emerging as early biomarkers for neurodegenerative risk stratification
See how our work drives better patient outcomes.
Inflammatory Bowel Disease: Remission Isn’t the Whole Story
Many IBD patients report persistent GI symptoms even during clinical remission. Understanding when symptoms are functional versus inflammatory is critical to optimizing care.
Practice-driven observations:
Patients in remission frequently report persistent discomfort not linked to active inflammation
Behavioral tracking at Penn Clinical identifies functional pain drivers, reducing unnecessary biologic escalation
Early functional profiling decreases steroid and immunosuppressant reliance in complex IBD populations
Inflammatory Bowel Disease: Remission Isn’t the Whole Story
Many IBD patients report persistent GI symptoms even during clinical remission. Understanding when symptoms are functional versus inflammatory is critical to optimizing care.
Practice-driven observations:
Patients in remission frequently report persistent discomfort not linked to active inflammation
Behavioral tracking at Penn Clinical identifies functional pain drivers, reducing unnecessary biologic escalation
Early functional profiling decreases steroid and immunosuppressant reliance in complex IBD populations
Gastroparesis: Neurological Links in Focus

Gastroparesis: Neurological Links in Focus
Gastroparesis is increasingly linked to early neurodegenerative processes, yet often goes undetected in the initial stages. Early identification changes the trajectory of care.
Findings from integrated care models:
- Delayed gastric emptying is common in neurological disease and often missed without early screening
- Early detection at Penn Clinical supports optimized medication and nutrition planning
- Gastric motility tracking improves coordination across GI and neurology teams
- Breath-based gastric emptying tests offer less invasive diagnostics for early-stage intervention
Mood Disorders with GI Symptoms
Mood disorders frequently overlap with GI distress, but standard GI or psychiatric approaches alone often miss cross-system patterns. Layered tracking improves differentiation and outcomes.
Clinical integration demonstrates:
Structured diet and neuromodulators demonstrate benefit in anxiety-driven GI symptom flares
Cross-tracking at Penn Clinical improves differentiation between psychogenic and organic symptom sources
Combined dietary-behavioral programs enhance sustained symptom resolution
Mood Disorders with GI Symptoms
Mood disorders frequently overlap with GI distress, but standard GI or psychiatric approaches alone often miss cross-system patterns. Layered tracking improves differentiation and outcomes.
Clinical integration demonstrates:
Structured diet and neuromodulators demonstrate benefit in anxiety-driven GI symptom flares
Cross-tracking at Penn Clinical improves differentiation between psychogenic and organic symptom sources
Combined dietary-behavioral programs enhance sustained symptom resolution
Novel Real-World Tools
Novel Pathways
Traditional models often fail to capture the lived complexity of GI-neurological comorbidity. New pathways and AI tools at Penn Clinical enable novel real-world clinical tools with significantly higher response, retention, and disease optimization.
Resulted in new clinical trial implementations:
- Predictive dropout modeling enables adaptive engagement strategies in decentralized clinical trials
- Patient stratification using mood-symptom history improves trial design and cohort targeting
- Machine learning models inform dynamic allocation into diet vs. neuromodulator intervention arms
- Real-world trial designs now reflect patient lived experience, not idealized protocols
Cross-System Therapeutics
When GI, neurological, and emotional symptoms interact, first-line therapies often fail. Cross-system therapeutics offer new frontiers for patients previously lost between specialties.
Patients with co-occurring anxiety and GI pain show stronger response to centrally acting agents
Symptom tracking informs the use of neuromodulators versus traditional GI therapies
Longitudinal outcomes support early use of cross-system agents in complex patients
Patients with co-occurring anxiety and GI pain show stronger response to centrally acting agents
Symptom tracking informs the use of neuromodulators versus traditional GI therapies
Longitudinal outcomes support early use of cross-system agents in complex patients
Why This Matters
These outcomes reflect more than symptom relief—they are reshaping how multisystem conditions are diagnosed, managed, and studied.
From early pattern recognition to precision-guided intervention, work at Penn Clinical is building the future of multisystem care:
- Earlier targeting of interventions.
- Better matching of therapies to symptom dynamics.
- Smarter systems built around patient complexity, not disease simplicity.
Every data point moves care closer to where it needs to be—for patients, for clinicians, and for the future of medicine.